Introduction
The two HOS outcome measures, Improving or Maintaining Physical Health (C04) and Improving or Maintaining Mental Health (C05) are moved to display for 2022 and 2023 Star Ratings1. The CMS memo from Amy Larrick Chavez-Valdez, Director of Medicare Drug Benefit and C & D Data Group, published on August 5, 2021, was a result of continuous undermining effects from the COVID-19 pandemic on these two measures.
With the absence of the two outcomes measures and other measures planned to be retired or moved to the display page, there continues to be a large and continued shift towards Member Experience2 Star measures as we march towards the 4x weighting in 2023.
Interestingly, the guidance did not explicitly mention removing these measures permanently but rather moving them to the display page. This article highlights implications health plans need to consider with this change.
Discussion and Impact
The two HOS measures being retired – Improving or Maintaining Physical Health (C04) and Improving or Maintaining Mental Health (C05) – signal CMS’ continued focus and concern about the COVID-19 pandemic effects. These two measures historically have been measured through the HOS survey. C04 measures the percent of plan members whose physical health was the same or better than expected after two years; C05 measures the percent of plan members whose mental health was the same or better than expected after two years.
The 2022 ratings would have covered data from the Medicare HOS 2018 Cohort 21 Baseline and 2020 Cohort 21 Follow Up surveys. It is well established that the pandemic disproportionately impacted seniors with higher death rates3, increased rates of loneliness4, increased depression5 and anxiety6, and decreased activity levels7. 2020 surveys measuring health improvement may be artificially skewed downward due to the unprecedented health impact of COVID-19.
These two Stars–both with a 3x weight–accounted for 4% of the Star Rating, so any decline in rating driven by reported deterioration in physical and mental health between 2018 and 2020 would have impacted a plan’s ratings.
In addition to C04 and C05, the following are changes coming in 2022 and 2023:
With these changes, there is an increase in the percent of Star Ratings attributable to the Member Experience measures (half of which are derived from the CAHPS survey). Before the 2022 changes, the Member Experience measures accounted for 37% of Star Ratings. The removal of the above measures boosted the importance, with Member Experience measures now accounting for 43% of all measures.8
Approaching the 2023 Star Ratings, changes to the ratings continue, the most significant of which is the Member Experience measures moving to a 4x weight listed below:
| C17 | Getting Needed Care | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| C18 | Getting Appointments and Care Quickly | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| C19 | Customer Service | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| C20 | Rating of Healthcare Quality | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| C21 | Rating of Health Plan | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| C22 | Care Coordination | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| C23 | Complaints about the Health Plan | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| C24 | Members Choosing to Leave Plan | Patients’ Experience and Complaints Measure | 2 | 2 | 4 |
| C26 | Plan Makes Timely Decisions about Appeals | Measures Capturing Access | 2 | 2 | 4 |
| C27 | Reviewing Appeals Decisions | Measures Capturing Access | 2 | 2 | 4 |
| C28 | Call Center – Foreign language Interpreter and TTY Availability | Measures Capturing Access | 2 | 2 | 4 |
| D01 | Call Center – Foreign Language Interpreter and TTY Availability | Measures Capturing Access | 2 | 2 | 4 |
| D02 | Complaints about the Drug Plan | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| D03 | Members Choosing to Leave the Plan | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| D05 | Rating of Drug Plan | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
| D06 | Getting Needed Prescription Drugs | Patients’ Experience and Complaints Measure | 1.5 | 2 | 4 |
In 2023, with the Star Rating removals, temporary suspensions, and additions, the Member Experience measures will account for 60% of the ratings9. There has been significant focus on the impending 4x Member Experience weighting change, and the accelerated removal of the C04 and C05 ratings continue the upward and more immediate trend in Member Experience and CAHPS measure importance. The impact of this change can be seen in the table with the weighted measures:
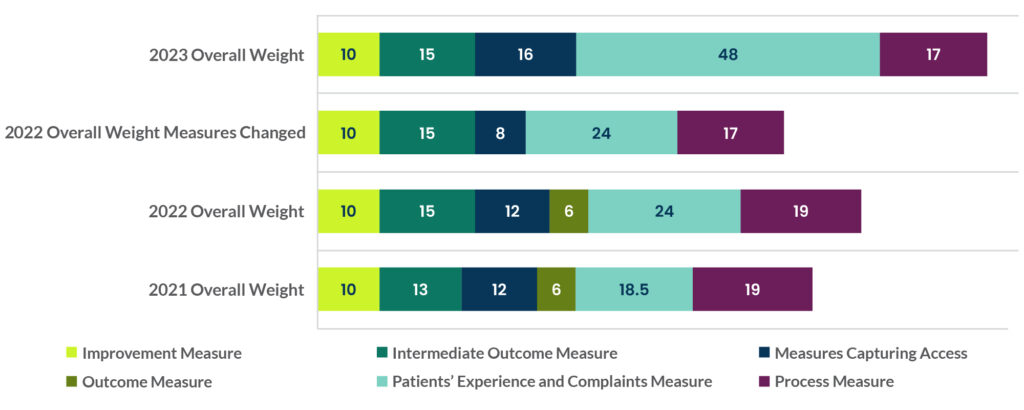
Graphic Description
This graph displays the modifications to the Star Ratings from 2021 to 2023, with the greatest increase of weighting (4x) added to the Patient’s Experience and Compliant Measure. Also, note the removal of the C04 and C05 measures as they are moved to the display page.
Any change in the Star Ratings, especially the removal or addition, will impact the role and importance of the Member Experience Star Ratings. It’s important to continue to evaluate how to maintain or improve these measures since they are the key components driving Star Rating performance.
In addition, until CMS permanently removes the HOS measures as a Star Rating, plans should consider continuing to survey its membership. If and when these measures are removed from the display page, plans will need to understand how its members are reporting health outcomes so that they can start to measure improvement or decline and implement programs and services that address these changes.
1 Chavez-Valdez, A. L. (2021, August 5). Medicare Health Outcomes Survey (HOS) Outcome Measures Moved to Display for 2022 and 2023 Star Ratings. Department of Health & Human Services Centers for Medicare & Medicaid Services. https://www.hosonline.org/globalassets/hos-online/hos_measures_852021.pdf.
2 This encompasses those weighting categories classified as “Patient experience and complaint measures” and “Measures capturing access”, half of which are evaluated using the CAHPS survey.
3 Centers for Disease Control and Prevention National Center for Health Statistics. Provisional Death Counts for Coronavirus Disease 2019 (COVID-19). COVID-19 Mortality Overview. 2021.
4 Krendl, A.C.; Perry, B.L. The Impact of Sheltering in Place During the COVID-19 Pandemic on Older Adults’ Social and Mental Well-Being. J. Gerontol. Ser. B 2020.
5 Krendl, A.C.; Perry, B.L. The Impact of Sheltering in Place During the COVID-19 Pandemic on Older Adults’ Social and Mental Well-Being. J. Gerontol. Ser. B 2020.
6 Chen, A. T., Ge, S., Cho, S., Teng, A. K., Chu, F., Demiris, G., & Zaslavsky, O. (2021). Reactions to COVID-19, information and technology use, and social connectedness among older adults with pre-frailty and frailty. Geriatric nursing (New York, N.Y.), 42(1), 188–195. https://doi.org/10.1016/j.gerinurse.2020.08.001
7 Schmidt T and Pawlowski CS (2021) Physical Activity in Crisis: The Impact of COVID-19 on Danes’ Physical Activity Behavior. Front. Sports Act. Living 2:610255. doi: 10.3389/fspor.2020.610255
8 CAHPS, which is a subset of Member Experience, accounts for 20% of all measures before the 2022 measure removal, and 23% after.
9 CAHPS alone will account for 31% of all Star ratings.

Still looking for more of the latest insights on health action?
Sign up for our newsletter so you never miss a thing!


